As Great Lakes communities begin easing up on physical distancing, a group of scientists is peering into the bowels of our cities and towns for signs of potential flare-ups.
Throat swab tests for the coronavirus are expensive and we aren’t capturing enough data for a true picture of how many people are infected, say epidemiologists.
But testing feces pulled from wastewater treatment plants may give us an early warning of infection spikes. Public health officials could use this information to decide whether to reintroduce physical distancing or boost hospital capacity.
“The so-called second and third waves we keep hearing about – we could see it (in sewage) maybe a week to 10 days before you start seeing manifestations of reinfection in the community,” said Mike McKay, an environmental microbiologist at the University of Windsor.

University of Windsor Professor Mike McKay. (Photo courtesy of University of Windsor)
Studies show the virus can be detected in infected people’s feces – sometimes even before they begin exhibiting symptoms. While we are still learning about COVID-19, researchers think the virus is no longer infectious by the time it reaches sewage treatment plants. But its genetic material remains intact enough to read its sequence and identify it.
McKay is teaming up with staff at two Ontario wastewater treatment plants to collect weekly samples of untreated sewage. The plants, in Lakeshore on Lake St. Clair and in Amherstburg, near the mouth of the Detroit River, process wastewater for roughly 50,000 people.
McKay expects to begin collecting samples before the end of May and hopes to have results showing trends in viral loads by mid summer.
Global effort
McKay is part of a group of researchers around the world, including in the United States, Europe and Australia, who are looking for the coronavirus’s genetic signature in sewage. They can’t determine how many people might be infected in a given catchment area, but they can detect a rise or fall in the viral load.
“However, because of the “stickiness” of the viral material, the decline in the signal will be slower than the rise in the signal,” said John Norton, director of Energy, Research & Innovation for the Great Lakes Water Authority in Detroit. “Basically, we expect the viral particles to stick to other organic materials in the sewer.”
The GLWA provides sewer service for about 2.8 million people in southeast Michigan, including those in Wayne, Oakland and Macomb counties. Its staff began collecting twice-weekly wastewater samples on April 7. They run the wastewater through a special filter cartridge, seal the filter in a zip-lock bag, put it on ice and send it to Michigan State University for laboratory analysis.
It’s not the first time MSU scientists have gone looking for viruses in sewage. In early 2018, environmental engineer Irene Xagoraraki identified an outbreak of hepatitis A about a week before reported cases.
As expected, MSU researchers have already identified coronavirus genes in the current sewage samples. They, along with other researchers in the region, are now refining their sampling and data analysis techniques to accurately reflect trends in infection.
“Everything we’re doing is at the research level at this point,” Xagoraraki said in a news release. “However, it could be part of a larger solution across the country and the world.”
Avoiding misleading results
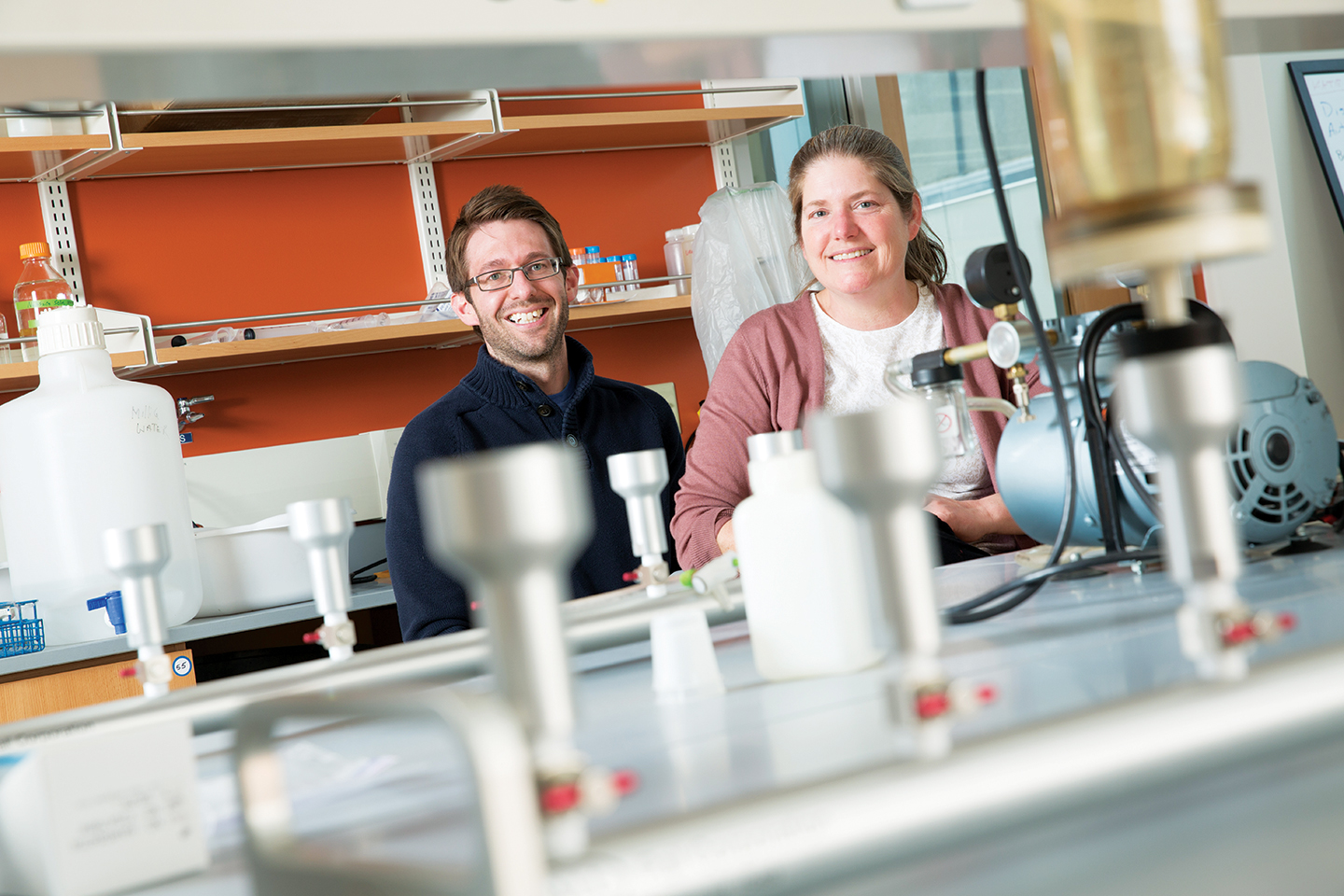
Ensuring sampling methods and analysis leads to useable results is not simple, warned Sandra McLellan, an environmental microbiologist at the University of Wisconsin-Milwaukee.
A sample from one area of sewage might show 20 “hits” for the virus, while a sample from another area of the same sewage pool might yield 200. A tissue from an infected person flushed down a toilet could be enough to boost the viral signal in the second sample, but it would not necessarily reflect a spike in infection.
“It may take some time to nail down how precise some of these methods are,” said McLellan. “I think generating data won’t be delayed, but we should be cautious about interpreting until we really have some time – months, not years – to dig into it.”
McLellan is working with the Milwaukee Metropolitan Sewerage District to collect samples twice a week from roughly a million people from Milwaukee and surrounding communities.
While she hopes to have a general idea of infection trends within a few weeks, McLellan stresses that sewage sampling should not replace the more traditional throat swab tests.
“We still need that,” she said. “But sewage testing does something traditional testing can’t do – give you a wide survey of your entire population. Right now, we’re blind. Even as a microbiologist, I don’t have an accurate idea of community infection.”
Featured image: University of Wisconsin-Milwaukee School of Freshwater Sciences researchers Ryan Newton and Sandra McLellan are organizing a regional effort to engage sewerage districts to monitor wastewater to spot coronavirus. It could be an early warning sign of disease in the community. (Photo courtesy of UWM Photo/Troye Fox)